It doesn’t get much more serious than being given the diagnosis that you have a brain tumor. Though brain cancer is rare and may be a life-threatening situation when detected, many forms of tumors can be successfully treated.
A brain tumor is a collection, or mass, of abnormal cells growing in, or next to the brain. But, what are the different types of brain tumors, and what are the symptoms to look out for?
Brain Tumor Symptoms
There are so many different types of brain tumors, and because each is so complex, brain tumors can cause different effects for each person. Physical problems and behavioral changes can occur throughout the body severely impacting one's life. The symptoms will depend on the individual's particular tumor, its location, and can result in:
- Drowsiness
- Personality changes
- Confusion
- Impulsiveness
- Blurred vision
- Balance problems
- Headaches
- Nausea
- Vomiting
- Seizures
Types of Treatable Brain Tumors
Though there are many different types, a brain tumor is classified by where it was originally formed. If it originated in the brain, it’s called a primary tumor and can be either noncancerous (benign), or cancerous (malignant). A tumor that originates in another part of the body and travels to the brain is called a meta tumor, and they are always cancerous.
Metastatic Brain Tumors - Also known as secondary tumors, they originate outside of the brain in another part of the body and then spread to the brain.
Meningiomas - Originating in the meninges, these thin layers of protective tissues surround the brain and spinal cord. Meningiomas usually grow slowly and most are not cancerous.
Pituitary Tumors - Found just under the brain, the pea-sized pituitary gland makes hormones that affect many of the body’s functions. A pituitary tumor can cause it to release too much, or too little, of these hormones which can cause serious problems.
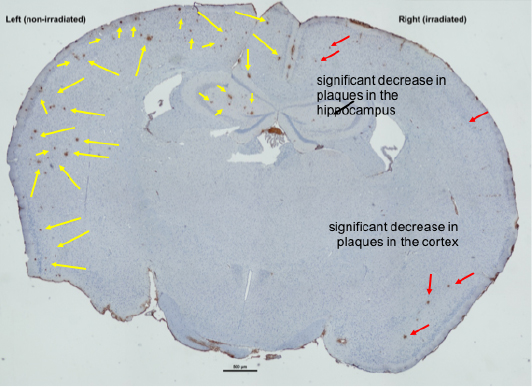
Glioblastoma Multiforme - These are the most challenging forms of brain tumors to treat. MHSI physicians have access to the most current technology to deal with this cancer including image-guided surgical treatments.
Schwannoma - The most common type of benign peripheral nerve tumor in adults and rarely cancerous. When schwannoma grows larger, it can make removal more difficult. This type of nerve tumor can occur in any part of the body, and at any age.
Keith’s Brain Tumor Story
Before Keith, a patient at Michigan Head and Spine Institute, was diagnosed with his brain tumor he was an accomplished musician hoping for a big break.
“I got my first guitar when I was 12. It’s what calms me. It’s where I can focus on one thing and the thousand thoughts going on in my head will go away.”
But, that was all about to change when he started experiencing unexplained health problems and physical ailments.
“The first symptoms I had were the nausea, dizziness and headaches,” he said, “It got to the point where I couldn’t eat. The only thing that was staying down was water.”
Knowing something was wrong with his health, he went to an emergency room hoping it was just an ear infection. After undergoing some tests, his ER doctor came back with unsettling information.
“A brain tumor was not on my list.” - Keith, a patient at MHSI
Diagnosed with a sporadic case of hemangioblastoma, a benign tumor, Keith was seen by Michigan Head and Spine Institute, trusted experts for treatment and diagnosis of tumors, diseases and other conditions of the brain.
After reviewing his CT scan, it was confirmed Keith had a large mass at the back part of the head in the region of the cerebellum. This part of the brain also contributes to coordination.
“I just wanted it to stop hurting, to stop feeling sick,” Keith recalled.
While being prepped for surgery he also remembered the last thing he told the anesthesiologist, “I said, ‘I’m a musician.’ When I came back out, I still wanted to be a musician.”
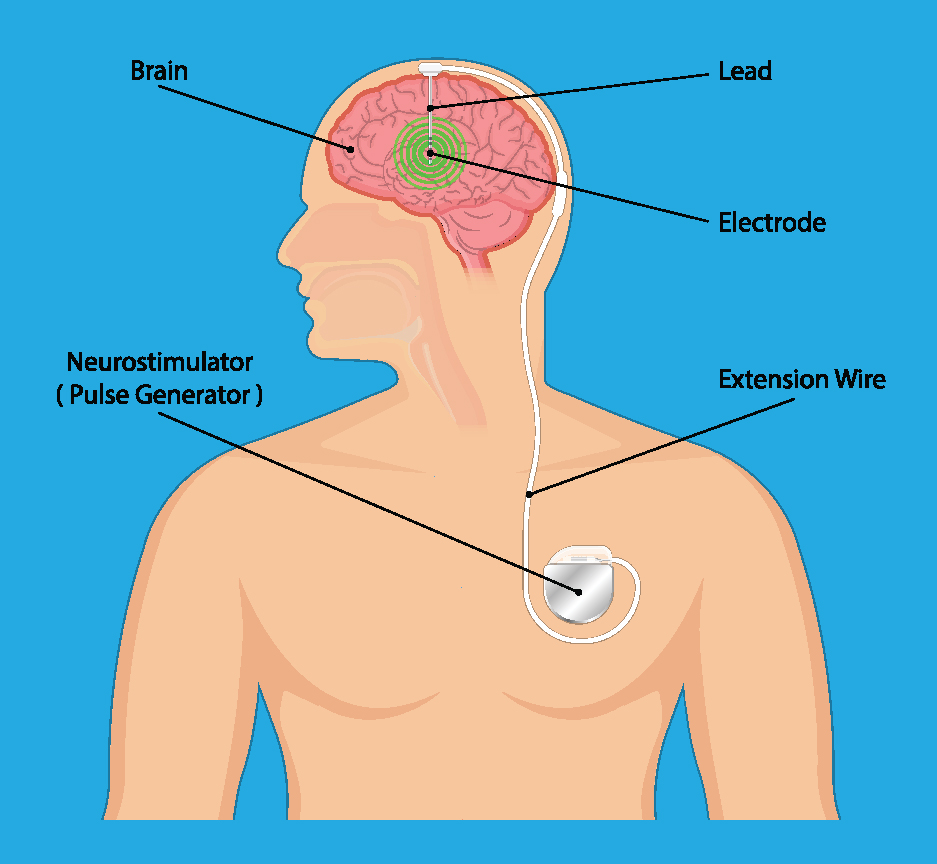
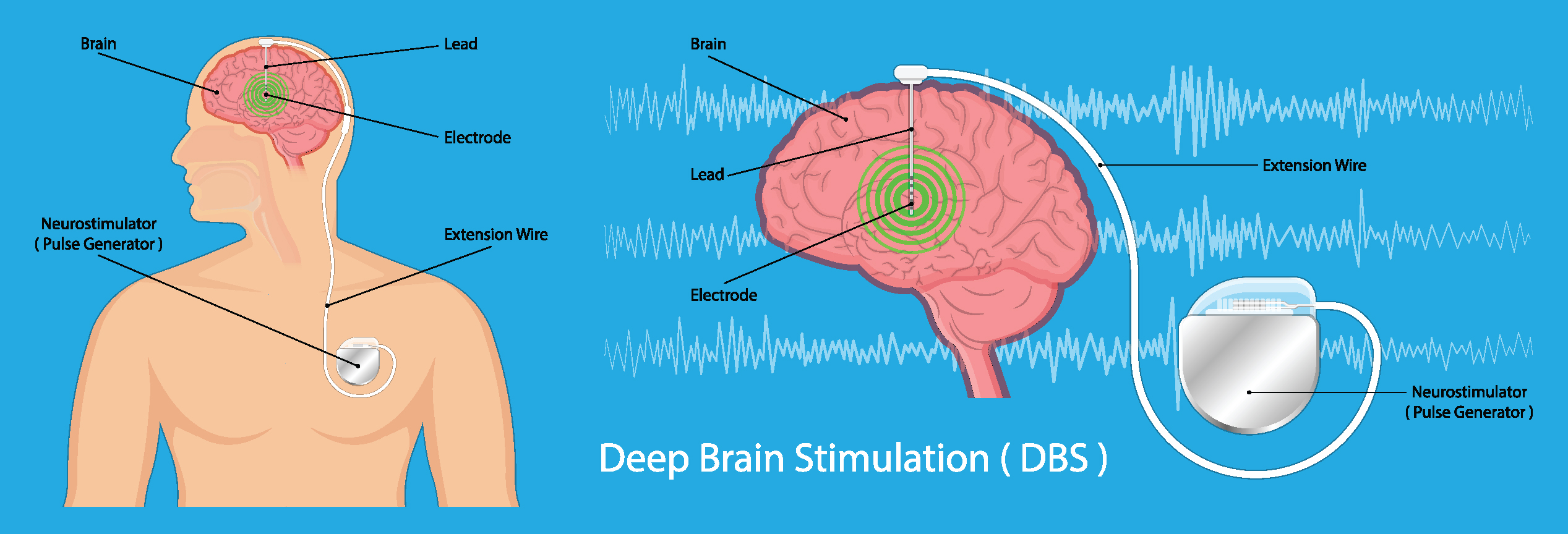
Keith’s surgery was successful. He then underwent a second nonsurgical procedure called Gamma knife treatment to remove the last bit of his tumor.
“When I woke up after the surgery, I knew it was fixed. The pain I was having before was gone,” he said relieved, “I like the way my doctor had a very confident way about himself.”
As for Keith’s guitar playing and music career after his surgery at MHSI:
“I’ve been in a few bands, had a little stardom,” he updated, “I’ve met a lot of people in the industry since the surgery that say they’re going to help me, so we’ll see what happens.”
To learn more about conditions of the brain and brain tumor procedures, please visit our MHSI Patient Education page at: Conditions of the Brain.
If you or a loved one is seeking treatment for a condition of the brain, or are seeking a second opinion on an existing diagnosis, schedule an appointment online or contact MHSI at 248-784-3667.
To view more information about MHSI’s neurosurgeons, visit: https://www.mhsi.com/doctors/neurosurgery-physicians/. For more information about MHSI’s neurologists, visit: https://www.mhsi.com/doctors/neurologists/